A Deep Dive into Cognitive Behavioral Therapy for Insomnia
Summary of a podcast by Dr Peter Attia and Ashley Mason
Introduction
Ashley Mason, PhD, is an Associate Professor at UCSF, leading the Sleep, Eating, and Affect (SEA) Lab and directing the COAST Center. Her work focuses on non-pharmacologic treatments for mood, sleep, and eating disorders, with a central focus on cognitive behavioral therapy for insomnia (CBT-I). In a conversation that serves as a master class, Dr. Mason breaks down the science, structure, and strategies of CBT-I—an intervention she champions as life-changing and highly effective.
What Is Insomnia?
• Definition: Chronic sleep issues persisting >3 months, causing distress or functional impairment.
• Prevalence: Affects 5–10% of adults at any time; 90% will experience it episodically.
• Diagnosis: No lab test—diagnosed clinically based on history and pattern.
The CBT-I Approach
Dr. Mason’s clinical model centers on five pillars:
1. Stimulus Control: Bed = sleep (and sex) only. No TV, phones, or reading.
2. Time in Bed Restriction: Match time in bed to actual sleep ability + 30 mins.
3. Cognitive Restructuring: Reframe catastrophic thoughts around sleep.
4. Relaxation Techniques: Focused body scans, progressive muscle relaxation.
5. Sleep Hygiene: Regulate light, temperature, caffeine, and bedtime habits.
How Insomnia Starts—and Stays
• Predisposing Factors: Genetic tendencies (e.g., light sleeper, high anxiety).
• Precipitating Events: Life stressors (divorce, job loss) trigger acute insomnia.
• Perpetuating Behaviors: Naps, sleeping in, screen use in bed, and inconsistent schedules prolong it.
Dr. Mason intervenes not at the origin, but at the behaviors keeping insomnia alive.
Tools and Tactics
• Scheduled Worry Time: Set a daily time to worry—offload anxiety from bedtime.
• Sleep Diaries: Track sleep patterns, test interventions, and calculate efficiency.
• A/B Testing: Isolate single variables (e.g., blue light glasses) for 2 weeks to test impact.
Key Sleep Hygiene Tips
• Consistent Wake Time: More critical than bedtime. No sleeping in.
• Temperature: Cool room (mid-60s°F); warm hands/feet to fall asleep.
• Fluid Intake: Reduce liquids after dinner to minimize night awakenings.
• Alcohol/Caffeine: No caffeine after 11 A.M.; no alcohol during CBT-I.
Medication and Supplement Use
• Avoid melatonin unless clearly indicated (e.g., beta blocker use).
• Eliminate sleep medications gradually with precision and physician support.
• Avoid rotating OTC and prescription meds—standardize and stabilize.
CBT-I Implementation at UCSF
• Program Structure: Intake → 5 weekly group sessions → follow-up.
• Group Format: 8 patients per cohort; group dynamic enhances adherence.
• Telemedicine: Fully remote access for California patients.
The Role of Digital Tools and AI
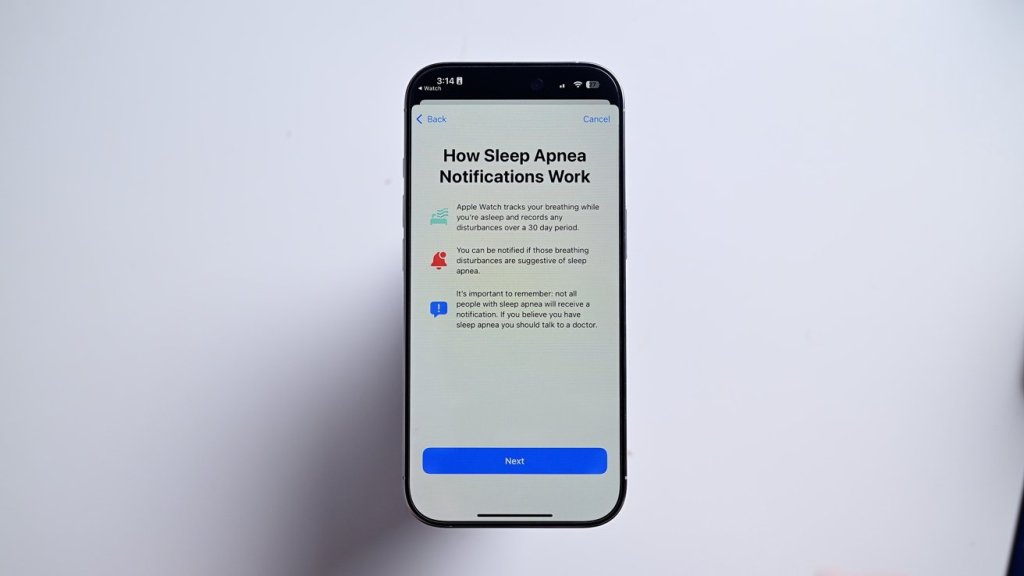
• Current apps show moderate promise, but personalization and accountability are challenges.
• Dr. Mason supports the development of AI-assisted programs (e.g., Rest) to democratize CBT-I.
Additional Sleep Disruptors to Rule Out
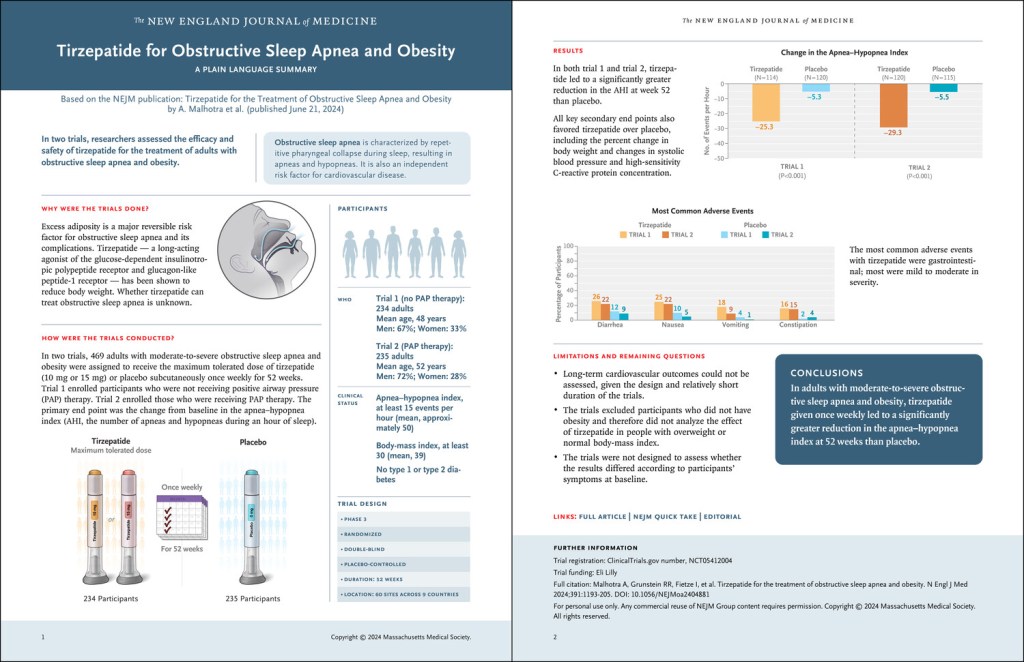
• Sleep Apnea / RLS: Screen and refer before starting CBT-I.
• Medication Side Effects: Some blood pressure meds suppress melatonin.
Practical Behavioral Advice
• Avoid Napping: Unless >80 years old, limit to 25 minutes max.
• Middle-of-the-Night Awakenings: Leave bed, do boring (non-stimulating) tasks until sleepy again.
• Social Jet Lag: Never sleep in two days in a row; choose which weekend day to feel rested.
Sleep, Anxiety, and the Cognitive Link
• Track belief in distressing thoughts across the day—most lose power by afternoon.
• CBT-I reframes distorted sleep-related beliefs, improving both sleep and mood.
Thermal Interventions and Future Research
• Sauna: May help some; trial shows promise combining heat therapy + CBT-I.
• Cold Plunge: Discouraged before bed—raises core temp post-exposure.
Takeaway
“You don’t have to know what caused your insomnia. Just do the treatment. It works when you do it.” – Dr. Ashley Mason
CBT-I is among the most effective psychological treatments available, with 70% of patients achieving clinically meaningful results. While adherence is essential, the payoff is substantial—better sleep, improved functioning, and often, life transformation. No one should have to suffer from insomnia. Access may be challenging, but tools exist—from books to digital apps—that can initiate recovery.
Recommended Resources
• Quiet Your Mind and Get to Sleep by Rachel Manber & Colleen Carney
• Sleep diaries (paper preferred)
• Society of Behavioral Sleep Medicine directory
• Rest (AI-supported CBT-I app in development)
Start now. It won’t be easy, but it will be worth it.