Short Audio Version: https://overcast.fm/+ABN64PpjuTY
Today we will explore the evolving landscape of dementia, with a particular focus on Alzheimer’s disease, Lewy Body dementia, and Frontotemporal dementia. Whether you are a clinician, caregiver, researcher, or someone navigating these conditions with a loved one, this episode aims to inform and empower.
We begin with the etiology of Alzheimer’s disease, a condition whose origins are multifactorial. The disease arises from a complex interplay of genetic predispositions, environmental exposures, and lifestyle factors. At the cellular level, the accumulation of amyloid-beta plaques and tau neurofibrillary tangles disrupts neuronal communication, triggers inflammatory responses, and ultimately results in widespread synaptic dysfunction and neuronal loss.
Additional contributors include chronic neuroinflammation, oxidative stress, and mitochondrial dysfunction. Genetically, while early-onset familial Alzheimer’s is rare and linked to a variety of mutations, the APOE ε4 allele remains the strongest risk factor for late-onset Alzheimer’s. Vascular pathology, sleep disturbances, diabetes, and poor cardiovascular health also play critical roles in disease onset and progression.
Lets consider the classification of dementia types. Alzheimer’s disease remains the most prevalent, accounting for approximately 60 to 70 percent of cases. Other types include vascular dementia, Lewy Body dementia, Frontotemporal dementia (FTD), mixed dementias, and less common conditions such as Creutzfeldt-Jakob disease and normal pressure hydrocephalus.
Frontotemporal dementia frequently presents between the ages of 45 and 65 and manifests with profound changes in personality, language, or behavior. It is commonly divided into three subtypes: behavioral variant FTD, primary progressive aphasia, and FTD with motor neuron disease or ALS. Familial inheritance is seen in a substantial number of cases.
In contrast, Lewy Body dementia typically affects individuals over the age of 65 and is characterized by fluctuating cognition, recurrent visual hallucinations, REM sleep behavior disorder, and parkinsonian motor features. These patients often exhibit severe sensitivity to antipsychotic medications, necessitating careful pharmacologic management.
In terms of diagnostics, the field is rapidly advancing. Biomarkers derived from cerebrospinal fluid, such as decreased Aβ42 and elevated phosphorylated tau, along with PET imaging for amyloid and tau pathology, now allow for earlier and more accurate diagnosis. Recently, FDA-approved blood-based tests like Lumipulse are improving access to non-invasive diagnostic tools. The A/T/N biomarker framework further enables clinicians to classify patients by underlying pathology rather than clinical symptoms alone.
Treatment options remain limited in terms of disease modification, but several monoclonal antibodies have demonstrated promise. Lecanemab and donanemab, for example, have shown statistically significant slowing of cognitive decline in early-stage Alzheimer’s patients. However, risks such as amyloid-related imaging abnormalities (ARIA) must be carefully managed. Ongoing trials are investigating additional compounds, including amyloid vaccines and anti-inflammatory therapies.
Living with dementia requires more than pharmacology, it demands a comprehensive care model. The GUIDE Program, a Medicare initiative launched in 2024, offers care navigation, caregiver support, and community-based resources. The program’s aim is to reduce caregiver burden, delay institutionalization, and improve quality of life through a structured, coordinated approach.
Finally, for those seeking support, numerous resources are available. These include memory care clinics, the Alzheimer’s Association’s 24/7 helpline, adult day centers, caregiver education, and long-term care planning services. Technology, such as wearable devices and smart home tools, can also enhance safety and independence.
This concludes today’s episode. For further information, please refer to the show notes for links to GUIDE, the Swank Memory Center, and biomarker updates. Thank you for listening and as always, we encourage you to stay informed and proactive in the pursuit of brain health.
Detailed Outline
ETIOLOGY
The etiology of Alzheimer’s disease (AD) is multifactorial and involves a complex interplay of genetic, environmental, and lifestyle factors.
🧠 Core Pathological Mechanisms
1. Amyloid-β Plaques
Accumulation of misfolded Aβ42 peptides leads to extracellular plaques.
These disrupt cell signaling, trigger inflammation, and may initiate synaptic dysfunction.
2. Tau Neurofibrillary Tangles
Hyperphosphorylated tau proteins aggregate inside neurons.
They impair microtubule transport and contribute to cell death.
3. Neuroinflammation
Chronic activation of microglia and astrocytes leads to neurotoxicity.
Inflammatory cytokines exacerbate neuronal injury.
4. Synaptic Dysfunction and Neuronal Loss
Caused by toxic oligomers, inflammation, and oxidative stress.
Leads to progressive cognitive decline.
🧬 Genetic Risk Factors
Early-Onset Familial AD (Rare, <1%)
Mutations in APP, PSEN1, or PSEN2.
Inherited in an autosomal dominant fashion.
Late-Onset AD (Common Form)
APOE ε4 allele is the strongest genetic risk factor.
Carriers have increased risk and earlier onset.
Other risk-related loci: CLU, BIN1, TREM2, PICALM, etc.
🔬 Other Contributing Factors
Mitochondrial dysfunction and oxidative stress
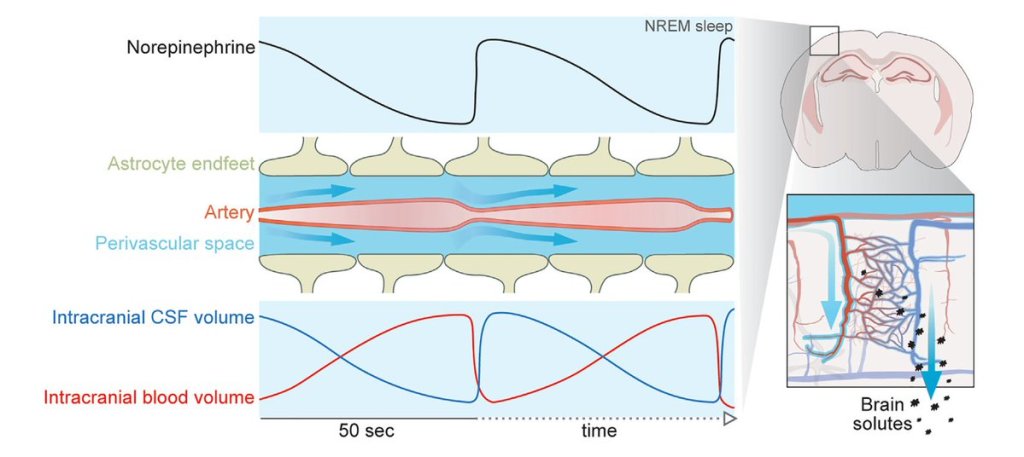
Impaired glymphatic clearance
Vascular disease and blood-brain barrier breakdown
Insulin resistance / Type 2 diabetes
Infections (e.g., herpes simplex virus, P. gingivalis — under investigation)
📊 Environmental and Lifestyle Influences
Head trauma
Low cognitive reserve (low education, social isolation)
Cardiometabolic risk factors (hypertension, obesity, diabetes)
Smoking, sedentary behavior, poor diet
Sleep disorders (especially sleep apnea)
Summary
Alzheimer’s likely results from a convergence of amyloid and tau pathology, neuroinflammation, genetic vulnerability, and lifestyle/environmental risk factors. Current research focuses on early biomarkers, disease-modifying interventions, and prevention strategies targeting modifiable risks.
TYPES
🧠 1. Alzheimer’s Disease (AD)
Most common type (~60–70%)
Caused by accumulation of amyloid-β plaques and tau tangles.
Key features: Memory loss, disorientation, language difficulties, impaired judgment.
Progression: Gradual and irreversible; begins with short-term memory impairment.
🧠 2. Vascular Dementia
Second most common; caused by reduced blood flow to the brain due to strokes or microvascular disease.
Key features: Stepwise decline, executive dysfunction, slowed thinking, focal neurological signs.
Often coexists with AD (“mixed dementia”).
🧠 3. Lewy Body Dementia (LBD)
Caused by alpha-synuclein (Lewy body) deposits in the brain.
Key features: Fluctuating cognition, visual hallucinations, parkinsonism, REM sleep behavior disorder.
Highly sensitive to antipsychotics (can worsen symptoms).
🧠 4. Frontotemporal Dementia (FTD)
Degeneration of frontal and/or temporal lobes.
Two main variants:
Behavioral variant: Personality change, disinhibition, apathy.
Language variants (Primary Progressive Aphasia): Non-fluent or semantic speech difficulties.
Younger onset (40s–60s) more common than other dementias.
🧠 5. Mixed Dementia
Combination of two or more types, often AD + vascular changes.
More common with increasing age.
Diagnosis often retrospective or at autopsy.
🧠 6. Parkinson’s Disease Dementia
Develops in patients with longstanding Parkinson’s disease.
Similar to LBD but motor symptoms precede cognitive ones.
Key features: Bradyphrenia, visuospatial deficits, apathy, hallucinations.
🧠 7. Normal Pressure Hydrocephalus (NPH)
Caused by impaired CSF absorption.
Classic triad: Gait disturbance, urinary incontinence, dementia (“wet, wobbly, and wacky”).
Potentially reversible with ventriculoperitoneal shunting.
🧠 8. Creutzfeldt-Jakob Disease (CJD)
Rapidly progressive, caused by prion proteins.
Key features: Myoclonus, ataxia, severe cognitive decline.
Prognosis: Typically fatal within months.
🧠 9. Other Rare Causes
Huntington’s disease
Chronic traumatic encephalopathy (CTE)
HIV-associated dementia
Autoimmune/paraneoplastic limbic encephalitis
Toxic/metabolic (e.g., alcohol-related)
Frontotemporal Dementia (FTD) is a group of neurodegenerative disorders primarily affecting the frontal and temporal lobes of the brain. It typically presents earlier than other dementias, often between ages 45 and 65, and is the second most common cause of dementia in people under 65.
🧠 Subtypes of FTD
1. Behavioral Variant FTD (bvFTD)
Most common type.
Symptoms:
Apathy, disinhibition, loss of empathy, socially inappropriate behavior
Poor judgment, impulsivity
Changes in eating habits or compulsive behaviors
Often mistaken for psychiatric illness (e.g., depression or bipolar disorder).
2. Primary Progressive Aphasia (PPA)
Language-dominant presentation, with two main subtypes:
Nonfluent/agrammatic variant (nfvPPA):
Halting, effortful speech
Impaired grammar and sentence construction
Semantic variant (svPPA):
Fluent but empty speech
Loss of word meaning and object recognition
3. FTD with Motor Neuron Disease (e.g., ALS)
Overlap of FTD symptoms with signs of motor neuron degeneration.
Rapid progression and poorer prognosis.
🧬 Causes and Genetics
30–40% of cases are familial with known gene mutations:
MAPT (tau)
GRN (progranulin)
C9orf72 repeat expansion (also seen in ALS)
Pathology may involve tau, TDP-43, or FUS protein accumulation, depending on subtype.
🔍 Diagnosis
Clinical assessment focused on personality, behavior, and language changes.
Neuroimaging (MRI/PET): Frontal and/or temporal lobe atrophy.
Genetic testing in familial cases.
Cognitive testing: May appear normal in early disease despite major functional impairment.
💊 Treatment
No cure or FDA-approved disease-modifying therapies.
Management is symptomatic:
SSRIs or trazodone for disinhibition or compulsive behavior.
Speech therapy for PPA.
Support for caregivers due to challenging behavioral symptoms.
Cholinesterase inhibitors (e.g., donepezil) used in Alzheimer’s typically not helpful and may worsen symptoms.
📉 Prognosis
Progressive and ultimately fatal.
Average survival: 6–11 years after symptom onset.
Faster progression with motor involvement.
Lewy Body Dementia (LBD) is a progressive neurodegenerative disorder characterized by the abnormal accumulation of alpha-synuclein protein (Lewy bodies) in the brain. It’s the second most common cause of dementia after Alzheimer’s disease, accounting for 10–15% of cases.
🧠 Key Clinical Features
1. Fluctuating Cognition
Marked variations in attention, alertness, and executive function.
Patients may appear lucid at times and profoundly confused at others.
2. Visual Hallucinations
Recurrent, well-formed, and detailed (e.g., people, animals).
Often occur early in the disease course.
3. Parkinsonism
Bradykinesia, rigidity, postural instability, and sometimes tremor.
May resemble idiopathic Parkinson’s disease, but typically follows or coincides with cognitive decline.
4. REM Sleep Behavior Disorder (RBD)
Acting out dreams during REM sleep.
Often precedes other symptoms by years.
5. Autonomic Dysfunction
Orthostatic hypotension, constipation, urinary incontinence, and temperature dysregulation.
6. Neuroleptic Sensitivity
Severe worsening of symptoms or life-threatening reactions to typical antipsychotics (e.g., haloperidol).
🧪 Diagnosis
Clinical criteria: Based on presence of core and suggestive features.
Neuroimaging:
Dopamine transporter (DaT) scan shows reduced striatal uptake.
Occipital hypometabolism on PET/SPECT.
MRI: May show less hippocampal atrophy than Alzheimer’s.
🔬 Pathophysiology
Lewy bodies (aggregates of misfolded alpha-synuclein) found in the brainstem, limbic system, and cortex.
Often coexists with Alzheimer’s pathology (amyloid plaques and tau tangles).
Cholinergic and dopaminergic deficits contribute to cognitive and motor symptoms.
💊 Treatment
Cognitive symptoms:
Cholinesterase inhibitors (e.g., rivastigmine) can improve cognition and reduce hallucinations.
Motor symptoms:
Low-dose levodopa may help but less effective than in Parkinson’s; may worsen hallucinations.
Behavioral symptoms:
Avoid typical antipsychotics.
If necessary, use quetiapine or clozapine with extreme caution.
Sleep and mood:
Melatonin or clonazepam for RBD.
SSRIs for depression/anxiety.
📉 Prognosis
Progressive and ultimately fatal.
Life expectancy: ~5–8 years from diagnosis.
Falls, aspiration pneumonia, and complications of immobility are common causes of morbidity.
🧬 Distinction from Related Disorders
LBD vs. Parkinson’s Disease Dementia (PDD):
In LBD, cognitive symptoms appear before or within 1 year of motor symptoms.
In PDD, motor symptoms precede dementia by more than a year.
FTD vs Lewy Body
🧠 Age of Onset
FTD: Typically 45–65 years
LBD: Typically over 65 years
🧠 Early Symptoms
FTD:
Personality change, apathy, disinhibition
Language deficits (in PPA variant)
Loss of empathy, poor judgment
LBD:
Fluctuating cognition
Visual hallucinations
Parkinsonism (rigidity, tremor, shuffling gait)
REM sleep behavior disorder
🧠 Memory Impairment
FTD: Often preserved early
LBD: Present early but fluctuates
🧠 Behavioral Changes
FTD: Prominent (socially inappropriate behavior, compulsivity, emotional blunting)
LBD: Less prominent initially; may develop later
🧠 Motor Symptoms
FTD: Usually absent early (except in FTD-ALS variant)
LBD: Parkinsonian features common and early
🧠 Hallucinations/Delusions
FTD: Rare
LBD: Common, especially visual hallucinations early in disease
🧠 Cognitive Fluctuations
FTD: Stable progression
LBD: Day-to-day or hour-to-hour variation in alertness and cognition
🧠 Response to Medications
FTD: May worsen with cholinesterase inhibitors
LBD: Cholinesterase inhibitors can help cognition and hallucinations
Extreme sensitivity to antipsychotics (may cause severe worsening)
🔬 Pathology
FTD: Tau, TDP-43, or FUS protein inclusions
LBD: Lewy bodies (alpha-synuclein aggregates)
🧬 Genetics
FTD: 30–40% familial; known mutations (MAPT, GRN, C9orf72)
LBD: Rarely familial; most cases sporadic
🧪 Imaging
FTD: Frontal and/or temporal lobe atrophy
LBD: Occipital hypometabolism on PET; relative sparing of hippocampus
📉 Prognosis
FTD: 6–11 years from symptom onset
LBD: ~5–8 years from diagnosis
DIAGNOSIS
🧠 Early Diagnosis: Faster, Less Invasive, More Accurate
1. Core CSF Biomarkers
These reflect the hallmark pathologies of Alzheimer’s disease:
Amyloid-beta 42 (Aβ42): Decreased levels in CSF indicate amyloid plaque deposition in the brain.
Total tau (t-tau): Increased levels reflect neuronal damage and degeneration.
Phosphorylated tau (p-tau, especially p-tau181 or p-tau217): Elevated levels correlate with tau tangles and are more specific to AD than total tau.
2. PET Imaging Biomarkers
Used to visualize pathology in vivo:
Amyloid PET (e.g., using florbetapir, florbetaben, or flutemetamol): Detects fibrillar amyloid plaques.
Tau PET (e.g., using flortaucipir): Detects paired helical filament tau deposits.
FDG-PET: Shows hypometabolism in the temporoparietal cortex, typical of AD.
3. MRI Biomarkers
Structural imaging to assess brain atrophy:
Medial temporal lobe atrophy, especially in the hippocampus, is characteristic.
Cortical thinning in the parietal and posterior cingulate regions can also be supportive.
4. Emerging Blood-Based 🩸 Biomarkers
More accessible and scalable than CSF or PET (LabCorp, Quest, Hospital)
Plasma Aβ42/Aβ40 ratio: Lower ratios may indicate amyloid pathology.
Plasma p-tau217: Show strong correlation with AD pathology.
FDA-approved blood test for amyloid detection
In May 2025, the FDA cleared the blood-based test
Fujirebio’s Lumipulse (pTau217, β‑Amyloid ratio)
5. Genetic Biomarkers
Used for risk assessment, especially in early-onset or familial cases:
APOE ε4 allele: Strongly associated with increased AD risk but not diagnostic.
Mutations in APP, PSEN1, PSEN2: Rare, associated with early-onset familial AD.
Biomarker Framework
The A/T/N classification is now used to describe biomarker status:
A: Amyloid (CSF Aβ42 or amyloid PET)
T: Tau (CSF p-tau or tau PET)
N: Neurodegeneration (CSF t-tau, FDG-PET, or structural MRI)
This framework helps stratify individuals by their underlying biology regardless of symptoms.
💊 Therapeutics: New and Emerging Options
Monoclonal antibodies targeting amyloid
1. Lecanemab (Leqembi)
•A large Phase III trial (Clarity AD) involving 1,795 participants with early Alzheimer’s disease showed a 27% slowing in clinical decline over 18 months versus placebo, with significant amyloid reduction verified by PET.
2. Donanemab (Kisunla)
•The TRAILBLAZER-ALZ 2 Phase III trial (1,736 individuals) reported a ~35% slower progression over 76 weeks based on composite scales (iADRS, CDR‑SB).
•Particularly, individuals with mild cognitive impairment experienced up to 60% slower decline on iADRS.
Update: New dosing schedule may reduce brain edema side effect (ARIA-e) https://cnmri.com/2025/07/14/fda-approves-label-change-for-alzheimers-drug/
3. Aducanumab (Aduhelm)
•Gained FDA accelerated approval in 2021, but its clinical benefit remains controversial due to inconclusive trial results and high adverse-event rates.
4. Next‑Generation Candidates
•Trontinemab (Roche) demonstrated rapid amyloid reduction—with 81% of patients reaching sub-24 Centiloid levels in just 28 weeks of Phase II data.
•Gantenerumab, though halted in general populations, showed benefit in genetically at-risk individuals in a 2025 study.
•TB006, targeting galectin‑3, recently showed promising Phase II results and ongoing Expanded Access in the US.
Clinical Significance & Caveats
•Meta-analyses confirm mAb therapies robustly clear amyloid and slow decline—but the clinical impact is moderate, and benefit may be questionable for late-stage or rapidly progressed cases.
•Adverse events, particularly ARIA (brain swelling/hemorrhage), occur in 15–40% of patients depending on agent and dosage.
Repurposed cancer drugs show promise
– A UCSF study found cancer drugs letrozole + irinotecan significantly reversed symptoms in Alzheimer’s mouse models.
– Analysis of patient records suggests lower Alzheimer’s prevalence among users, paving the way for clinical trials.
Pipeline developments
– Over 180 clinical trials are ongoing, exploring over 130 novel compounds targeting amyloid, tau, inflammation, and synaptic health.
– Investigational approaches include amyloid vaccines, secretase inhibitors, tau aggregation blockers, and saracatinib (a synaptic enhancer).
Innovative delivery methods
– Breakthrough research includes brain-implanted graphene devices and nasal vaccines aiming for targeted neural stimulation.
🌱 Symptom Management & Prevention
Cholinesterase inhibitors & memantine
– Standard treatments—donepezil, rivastigmine, galantamine, and memantine—continue to offer modest symptomatic relief; don’t halt neurodegeneration.
Lifestyle interventions
– Emphasis on heart-healthy habits: regular exercise, Mediterranean/MIND diet.
– Nutritional supplements, e.g. omega‑3, B‑vitamins, evidence mixed.
RESOURCES
🏥 Medical & Clinical Support
Neurology clinics – for diagnosis, medication management, and care planning.
Memory care centers – multidisciplinary teams focused on cognitive disorders.
Geriatric psychiatry – for behavioral symptoms like anxiety, agitation, or hallucinations.
Home health agencies – provide nursing, therapy, personal care services in the home.
🧭 Caregiver & Patient Education
Alzheimer’s Association (www.alz.org)
24/7 helpline: 1-800-272-3900
Dementia Friendly America (www.dfamerica.org)
National Institute on Aging (www.nia.nih.gov)
🤝 Support Groups & Counseling
In-person/virtual support groups for patients and caregivers.
Individual/family counseling – licensed therapists who specialize in aging.
Adult day centers – supervised environments for socialization, activities, respite.
🏡 Residential & Long-Term Care Options
In-home care aides – for activities of daily living (ADLs).
Assisted living with memory care units – secure environments with trained staff.
Skilled nursing facilities – for more advanced needs and medical support.
Hospice and palliative care – for late-stage support focused on comfort.
📄 Legal and Financial Planning
Elder law attorneys, for power of attorney, guardianship, wills, and Medicaid planning.
Financial planners, to manage long-term care funding, insurance, and asset protection.
Social workers/case managers – connect families with available benefits and programs.
🧘♀️ Technology & Daily Living Aids
GPS trackers, cameras (WYZE), Apple Watch, medical alert devices.
Medication reminders, automatic dispensers
Smart home tools – for lighting, appliances, and emergency response.
Memory aids – whiteboards, calendars, visual cues, labeled drawers.
💰 Financial Assistance
Medicare/Medicaid
Veterans Administration (VA) Aid & Attendance
State aging agencies and Area Agencies on Aging (www.n4a.org)
Long-term care insurance, if previously purchased.
GUIDE Program
The GUIDE Model (Guiding an Improved Dementia Experience) is an eight-year, voluntary Medicare initiative launched July 1, 2024, by the Centers for Medicare & Medicaid Services (CMS). It aims to enhance dementia care quality and support for patients and their unpaid caregivers through structured, coordinated services.
🧩 Core Components
1. Care Navigation: Each person with dementia and their caregiver is paired with a Care Navigator who provides ongoing support, care coordination, and access to community services and respite care.
2. Nine Required Service Domains: Includes comprehensive assessments (e.g., Clinical Dementia Rating), individualized care planning, 24/7 helpline access, regular monitoring, medication reviews, caregiver education, coordination with services, respite support, and specialist referrals.
3. Caregiver Education & Respite: Caregivers are provided training and structured respite services (e.g., adult day centers) to alleviate burden and delay institutionalization.
4. Alternative Payment Model: Instead of fee-for-service, participating providers receive a per-beneficiary monthly dementia care management payment (DCMP), adjusted for complexity, geography, caregiver presence, and performance.
🎯 Goals & Benefits
1. Keep patients at home longer and reduce unnecessary hospital or long-term care admissions.
2. Reduce caregiver strain via education, support, and respite resources.
3. Address social determinants of health by screening and connecting families to community resources.
4. Improve health equity, prioritizing underserved populations with performance-linked incentives.
🏥 Participation & Eligibility
Eligible providers: Medicare Part B-enrolled clinicians and health systems.
Two tracks:
Established programs start July 2024.
New programs go live July 2025 after a planning period.
Eligible beneficiaries:
Medicare Part A/B (non-Medicare Advantage),
Diagnosed with dementia (any stage),
Living in the community (not in nursing homes or hospice) .
Swank Memory Center (offices in Newark, Smyrna, Rehoboth)